Hysterectomies, Part 2 - Risks and Side Effects
In our last blog topic, ‘Hysterectomies, Part I - Here’s What You Need to Know’, we discussed some of the medical reasons why women may need to undergo a hysterectomy, as well as the different types. However, there are some dangers associated with this procedure that patients should be aware of when deciding whether or not to go forward with it.
Though a hysterectomy is an effective treatment for women dealing with a range of serious health concerns, it has also been associated with various risks and side effects. Many of these have been observed soon after the procedure, yet long-term outcomes are just now beginning to be researched.
This article will walk you through some of the dangers associated with hysterectomies and help you determine whether or not your condition results from medical malpractice.
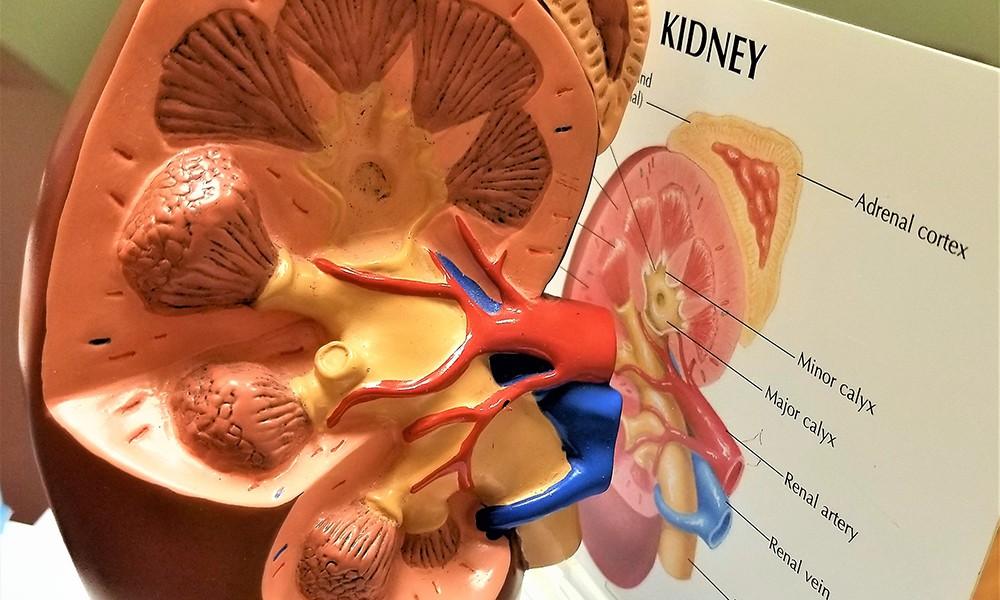
Hydronephrosis after a Hysterectomy
Hydronephrosis occurs when a patient experiences swelling in one or both kidneys. This swelling is typically a result of an obstruction or blockage in the drainage tubes connected to the kidneys (ureters), causing urine to build up within them. However, it can also occur when there is some other defect within the abdomen that prevents urine from draining out of the kidneys properly [1].
Side effects associated with hydronephrosis include:
- Aches or pains in the side, back, lower abdomen, or groin area
- Frequent or urgent need to urinate
- Urinary tract infections (UTI)
- Vomiting and nausea
- High fever
The Connection Between Ovary Removal and Chronic Kidney Disease
When someone has chronic kidney disease, also known as chronic kidney failure, their kidneys cannot operate or filter fluids as they should. If their kidney damage continues to deteriorate and the organ begins to fail, the only treatments available are dialysis and a kidney transplant.
If this kidney disease is left untreated or undiagnosed, it can result in the loss of organs, permanent injury, or even death.
Only recently have experts begun to acknowledge the significant correlation between estrogen insufficiency and kidney impairment, especially in premenopausal women. Because of this revelation, we now know that women whose ovaries have been surgically extracted are at a heightened danger of developing long-term kidney issues, including hydronephrosis [2].
Case Example: Undiagnosed Hydronephrosis After a Hysterectomy
To understand the full extent of the risks associated with hydronephrosis left undiagnosed, let’s look at one of our cases, the Balmene Case.
In this instance, carelessness in stitching up after a hysterectomy resulted in a blockage of the right ureter that was left undiagnosed and thus not addressed for five years. The patient first reported symptoms aligned with hydronephrosis as soon as two days after her hysterectomy, when her symptoms were so severe that she was admitted to the emergency room. Her doctors at the time persistently brushed off her concerns and refused to acknowledge the reality of her condition.
After five years of frequent UTIs, hypertension, blood in urine, chest pain, shortness of breath, pelvic pressure, and abdominal pain, among other symptoms, the patient’s changing health insurance policy caused her to see a new gynecologist. Immediately, the patient’s new doctor could tell that something was amiss and ordered several tests and treatments to address the issue.
It did not take long for the new gynecologist to identify the misplaced sutures that were causing the issue.
As a result of the negligence that took place in the five years following her initial surgery, the patient’s right kidney, ovary, and fallopian tube all needed to be removed.
Consequently, we represented the patient and filed a lawsuit against her gynecologist, primary care physician, radiologist, and the medical center where the operation was conducted.
Other Long-Term Dangers Associated With Hysterectomies
Despite hysterectomies being one of the most popular surgeries in the world, experts are still only just beginning to uncover the long-term conditions that can occur as a result of the surgery. Below are a few of the most common [3].
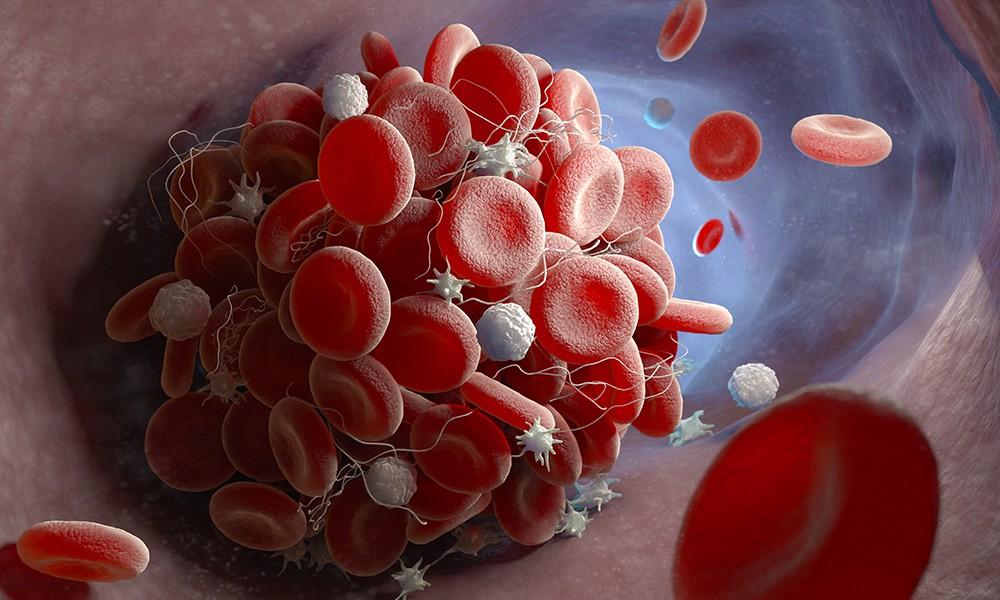
Deep Vein Thrombosis (DVT)
DVT takes place when a blood clot (thrombus) develops in deep veins in the body. In most cases, DVT starts in the legs. If left untreated, this condition can become more severe as blood clots will loosen and move through veins before lodging in the lungs, resulting in a pulmonary embolism (PE).
DVT is another common condition associated with hysterectomies. Research suggests that certain risk factors can heighten the patient’s risk of experiencing DVT post-operation [4].
You may be at a greater risk of experiencing DVT if:
- Your BMI is 35 or more
- You’ve had an Abdominal Hysterectomy
- You are in surgery for a longer period than expected
- You need a hysterectomy to treat gynecologic cancer
If it is caught early enough, DVT can be treated with compression bandages and anticoagulation treatments.
Unfortunately, some doctors tend to overlook the symptoms of DVT, resulting in severe repercussions for their patients.
Symptoms associated with DVT include:
- Leg pain
- Chronic swelling
- Pressure within veins
- Intensified pigmentation and discoloration
- Leg ulcers
Bowel Perforation
Bowel perforation is another risk associated with hysterectomies. This can occur when the surgeon knicks or cuts the bowel unintentionally. Surgery of the pelvic area can be a delicate operation, especially for inexperienced surgeons who may mistakenly damage the intestines when attempting to remove the uterus or other organs in the area. This risk is compounded by prior abdominal procedures, as well as conditions such as endometriosis, tumors, and large fibroids that can distort the anatomy of the pelvis.
The consequences of an untreated or improperly repaired intestinal injury during a hysterectomy can be severe. Fortunately, if bowel perforation is detected early, most individuals will make a full recovery with no other issues. Nonetheless, it is imperative for your surgeon to detect these kinds of injuries to avoid any long-term ramifications.
Patients who experience early signs of a perforated bowel following a hysterectomy may experience the following symptoms:
- Intense abdominal pain
- Fever
- Chills
- Nausea
- Swollen belly
Unfortunately, it is common for medical practitioners to disregard these warning signs as just being a regular part of the recovery period and disregard the patient’s grievances until the infection becomes more serious.
Are Hysterectomies Always Necessary?
The short answer to this is no. Surprisingly enough, research has revealed that 1 in 5 hysterectomies are considered unnecessary. However, the rate at which these operations have been conducted without necessary cause has decreased over time.
With that said, hysterectomies are necessary for many instances. Specifically treating various conditions, such as uterine fibroids, uterine prolapse, cancer, endometriosis, and others.
As more and more medical practitioners are opting in favor of avoiding hysterectomies, we have seen the rise of an alarming reality: women who need lifesaving hysterectomies are being instructed to avoid them.
This can pose a grave problem for patients down the line and is another example of medical malpractice or negligence.
Harry S. Cohen & Associates
Don’t face the hardships of a hysterectomy alone! Our supportive and knowledgeable team of professionals and attorneys are here to help you.
Call us at (412) 281-3000 or toll-free at 1-888-MEDMAL1 (1-888-633-6251) for your free consultation.
References
[1] - Hydronephrosis, Mayo Clinic
[2] - Ovary removal may increase risk of chronic kidney disease, Mayo Clinic News Network
[3] - What We Know about the Long-Term Risks of Hysterectomy for Benign Indication - A Systematic Review, National Library of Medicine
[4] - Risk Factors for Venous Thromboembolism After Hysterectomy, National Library of Medicine